harm reduction
12 |
drinkanddrugsnews
| June 2015
Progress on naloxone
distribution is still slow and
inconsistent throughout the
UK.
DDN
asked naloxone
champion Philippe Bonnet for
some tips on moving forward
A
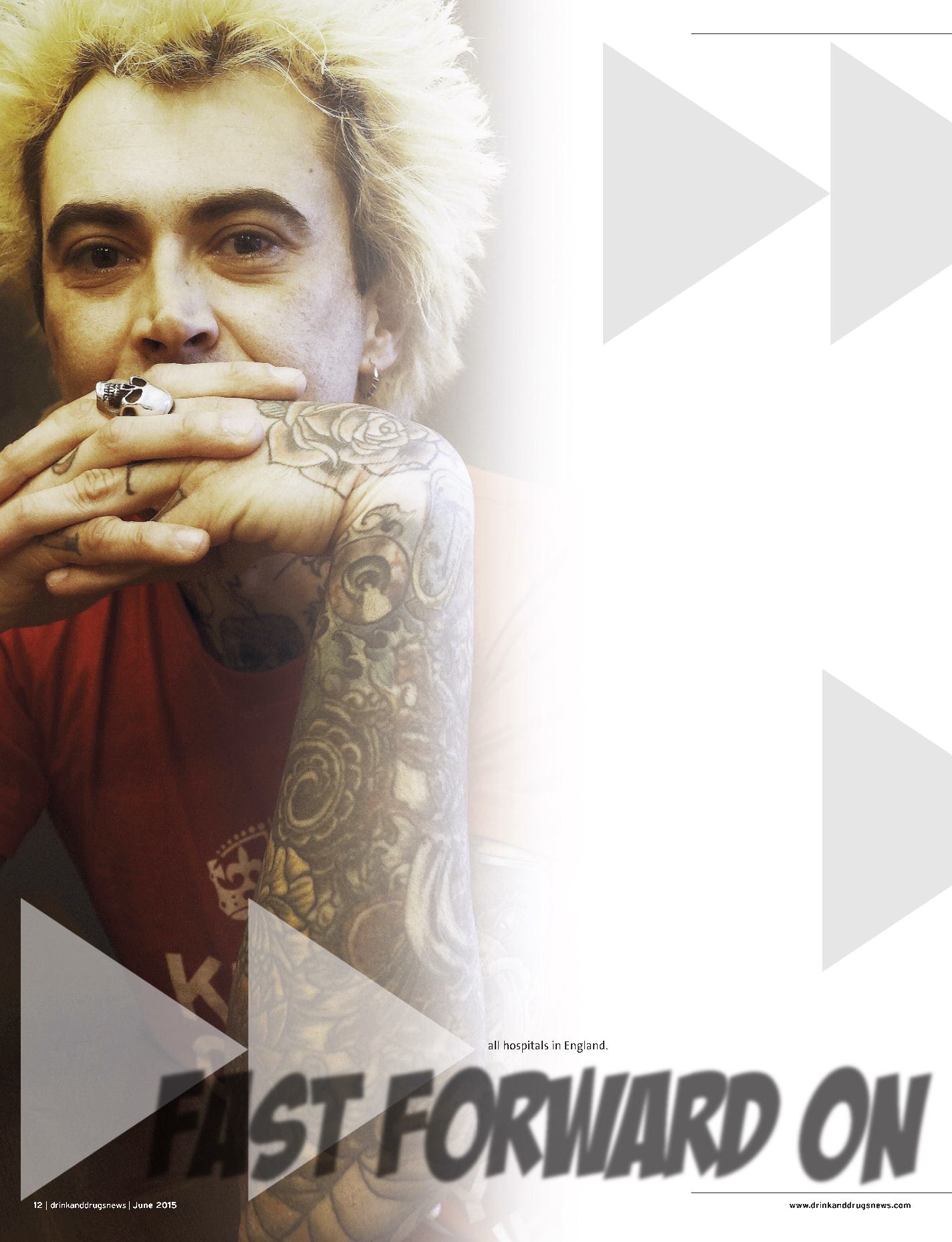
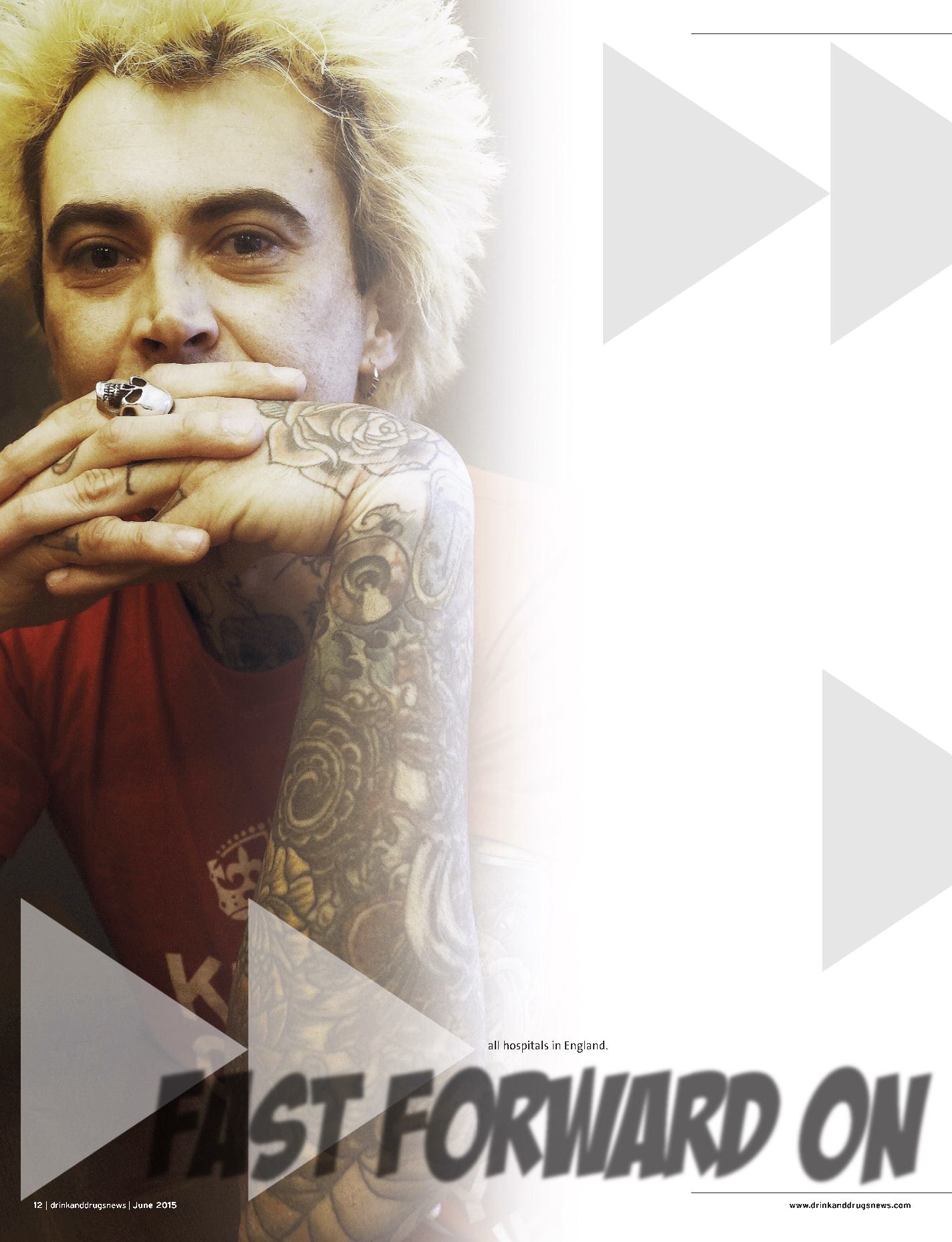
s part of a team committed to distributing naloxone, Philippe Bonnet
hears of an overdose being reversed every week in Birmingham. While
he credits a very active commissioner and a proactive treatment
provider for their role in making naloxone a central part of the area’s
drug strategy, he has learned some useful lessons over the past three years. As
chair of Birmingham’s naloxone steering group and Reach Out Recovery worker
at the sharp end of client care, he has experience worth sharing.
MAKE CHAMPIONS
‘What is key is to have real champions, who are going to be proactive,’ he says.
‘We identified champions from each service and told them their role was to get
to colleagues as well as clients – to get those kits out into the clients’ hands. It’s
no good just talking about it.
‘The staff can be trained in two hours, which covers who’s most at risk, myth
busting, overdose awareness and how to use the kit,’ he says. ‘They can then
train a client in five minutes. It’s so straightforward.’
CREATE A NETWORK
The support of local doctors makes life easier, says Bonnet. ‘We have a number of
doctors who are so pragmatic, very switched on. Dr Judith Yates was instrumental
from the beginning, not to mention many wonderful prescribing nurses.’
Another important partner is the local ambulance service – and there were
some barriers to tackle, he admits. Following an incident where paramedics
told a client off for using naloxone, Bonnet contacted the lead of the
ambulance service.
‘I couldn’t believe how pragmatic that guy was,’ he says. ‘The next day I had
an email saying a memo would be sent out to all the crews, telling them that in
Birmingham all drug users were being equipped with naloxone.’
The process had to be repeated with the 999 telephone operators, after one
of them told a caller from a hostel not to give naloxone to an overdose victim.
Bonnet drew a comparison with anaphylaxis – ‘would you tell them not to use
adrenaline?’ – and protocol for telephone operators is changing.
Discussions are still underway with the police to work out how initiatives
can be incorporated into protocol, but there has been progress with other local
partners, he says. Just weeks ago, HMP Birmingham gave the go-ahead for kits
on release.
Making sure hostel owners ‘understand the rationale and legislation around
naloxone’ has given many more confidence, knowing that ‘absolutely,
categorically, anyone can not only carry, but use, naloxone to save a life.’
Likewise, working with central Birmingham hostels that dealt with countless
overdoses led to training for the homeless treatment team of Dr Andrew
Thompson at a major hospital. ‘This is a major initiative and it’s early days,’ says
Bonnet. ‘The idea would be to give a naloxone kit following discharge from an
overdose or other drug-related admission – ideally this would be rolled out for
all hospitals in England.
Fast forward on