attaining abstinence in only 14 days. It also switched the client’s focus from the
detox process, to the real and more deserving challenge of maintaining abstinence
and recovery.
INCREASED VALUE
Aside from the clear benefits of our clients having an improved chance of actually
completing their detox, we found that running this model alongside the existing
alcohol detox service made better use of resources – both in terms of facilities
and staff. Having a programme that was time limited, with a clear beginning,
middle and end, also enabled us to plan aftercare services more effectively. We
also found that working alongside mutual aid groups such as SMART Recovery
and NA was an essential ingredient in the success of the model. Using our
existing relationships with our colleagues in community pharmacies helped to
add another layer of support.
WHO IS IT FOR?
As with cooking, a dish only suits some people but not others. ‘Detox in a box’ best
suits patients stabilised on methadone or buprenorphine, highly motivated to
detox in the community within a short period of time and with no major
psychiatric or physical health co-morbidities. It is unlikely to be successful for those
still using heroin exclusively or on top of methadone.
July/August 2016 |
drinkanddrugsnews
| 23
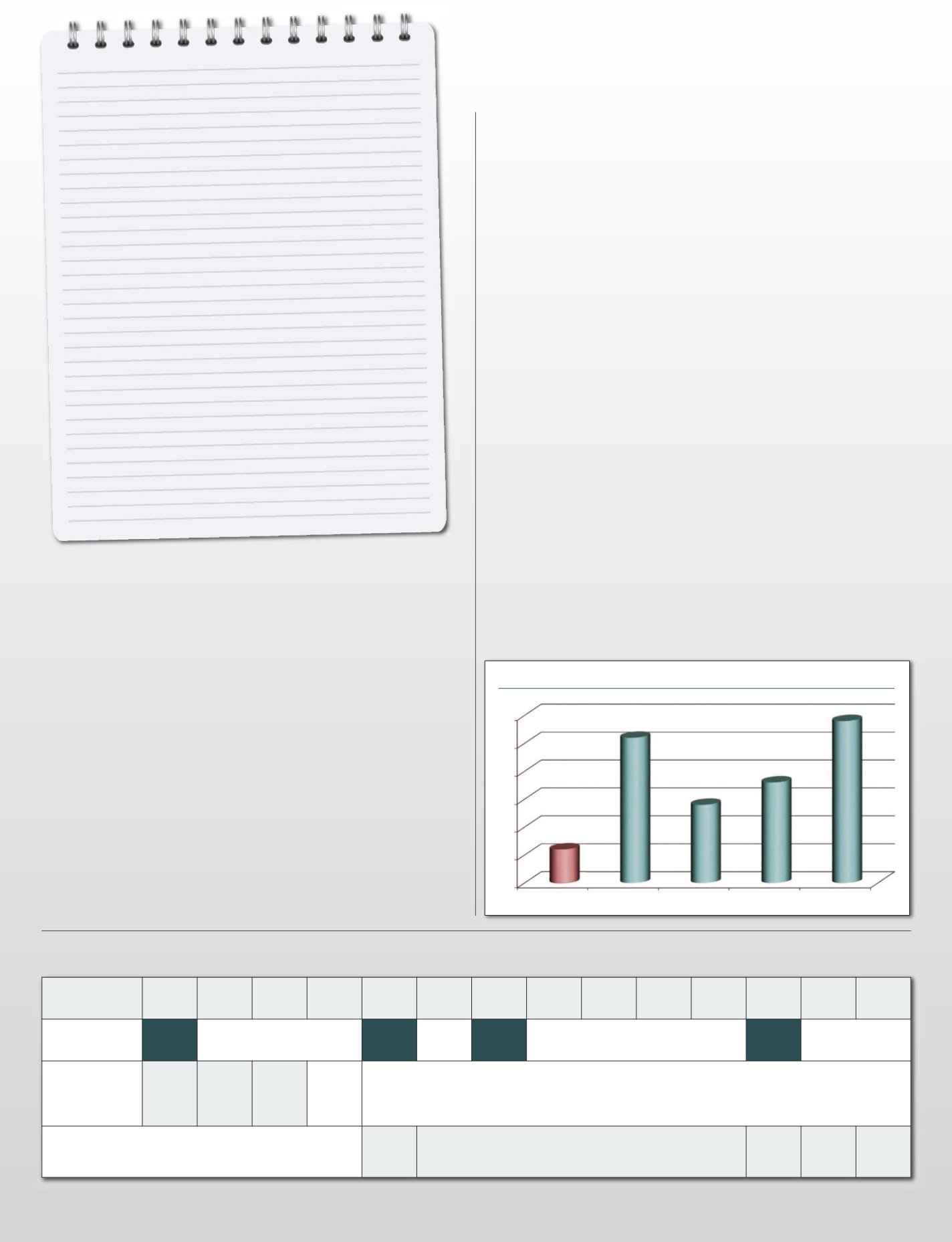
Number of patients exiting opiate-free from ‘detox in a box’ services
30
25
20
15
10
5
0
2010
2011
2012
2013
2014
‘Detox in a box’
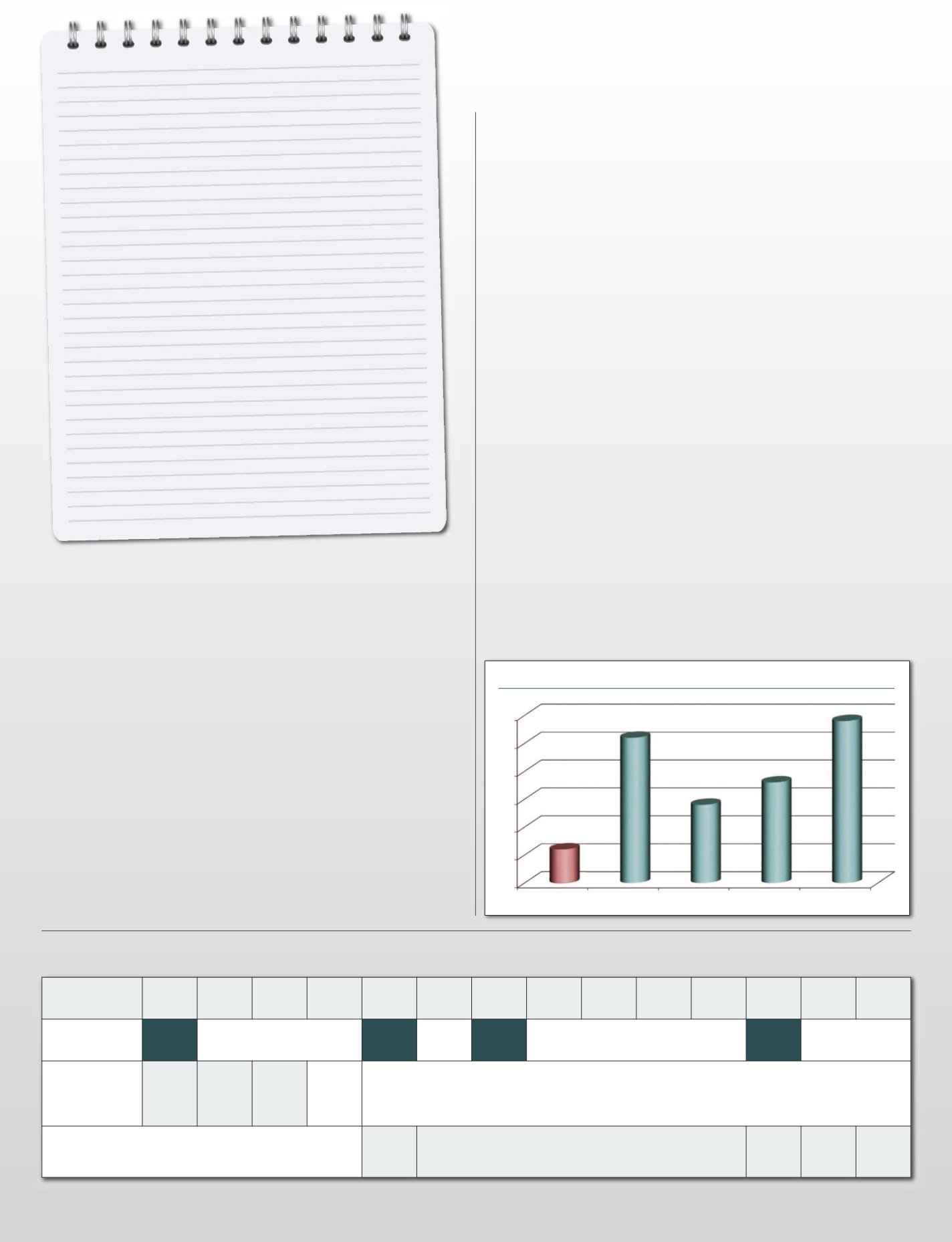
The recipe at a glance
• Ability to reduce to <40mls methadone
and transfer to buprenorphine
• Access to mutual aid support
• Only four outpatient visits needed
over 14 days.
• Buprenorphine front-loading (days 1-3)
• Lofexidine (days 5-14)
• Naltrexone offered day 12
(but not compulsory)
• Clear aftercare plan in place
DAY
1
Thurs
2
Fri
3
Sat
4
Sun
5
Mon
6
Tues
7
Weds
8
Thurs
9
Fri
10
Sat
11
Sun
12
Mon
13
Tues
14
Weds
Appointment
(seen in clinic)
Seen
Seen See Seen
Seen
Buprenorphine
8mg
(Split
dose)
16mg 8mg
With our buprenorphine front-loading protocol patients have a milder, slower withdrawal that onsets on or after
day 5 of detox (due to buprenorphine’s long half-life and high occupancy). Therefore, no lofexidine is needed until
day 5, and lower doses can be used with significantly reduced monitoring. Blood pressure only needs checking on
day 5 – the patient has a baseline, takes lofexidine and blood pressure is rechecked 30 minutes later.
Lofexidine
qds: four times a day
tds: three times a day
bd: twice a day
0.2mg
qds
0.2-0.4mg qds, for days 6 to 11
0.2mg
qds
0.2mg
tds
0.2mg
bd
outpatient opiate detox prescribing plan
CHALLENGES
Before implementing this approach, we were disheartened by the number of
service users who had been held on non-therapeutic doses of methadone and
buprenorphine for long periods of time, because of fear or anxiety about the opiate
withdrawal process. Their fears were further reinforced by a lack of confidence in
staff around the medications that could be prescribed or the psychosocial advice
that could be provided to help reduce the severity of the symptoms of opiate
withdrawal. In addition, we were faced with new challenges which included an
increased focus on treatment exits, compliance with our payment by results
targets, a staff culture that focused singly on maintenance treatment, a service user
expectation that engagement in psychosocial interventions was not required, and a
general fear of change.
Our greatest challenge during the implementation stage was our ability to
embed this approach as ‘treatment as usual’, alongside the slower reduction or
‘Russian doll’ approach that was more commonly used. Changing culture is often
the hardest thing we do in healthcare services and staff engagement in the process
was the key to ensuring the approach was owned by the service and offered to
service users. To our surprise we achieved this very quickly. Peer mentors were
involved from the start and their views adopted into the model; all staff members
were trained, and awareness sessions delivered to partnership agencies. Leaflets
were placed with all blank care plans, ready for discussion at the service users’ next
review appointment.
For us, it offered a fresh new treatment choice to add to the menu of options for
our service users who were looking to make significant behaviour change and
improve their lives.
About the authors:
R Iosub and I Seeger are senior registrars, South Gloucestershire and Bristol Specialised
Drug and Alcohol Services, Avon and Wiltshire Mental Health Partnership NHS Trust. F
D Law is consultant in substance misuse psychiatry at Turning Point. M Gilman is
managing director of Discovering Health. N S Wallbank is team manager at Stokes
Croft, Bristol Specialised Drug and Alcohol Services, Avon and Wiltshire Mental Health
Partnership NHS Trust. J K Melichar is medical director, DHI; medical director, DMT Ltd
and consultant in substance misuse psychiatry at Turning Point.