For the stories behind the news
February 2016 |
drinkanddrugsnews
| 9
see alcohol and ageing on the agenda across a
number of cross-care areas, such as dementia,
retirement, social isolation. Alcohol use
doesn’t happen in a vacuum.’
The programme is also advocating for the
needs of older people to be specifically
highlighted in existing government strategies,
in order to raise the issue in professional and
commissioning circles. ‘Up until now only the
Wales and Northern Ireland alcohol strategies
particularly reference the needs of older
adults,’ says Breslin.
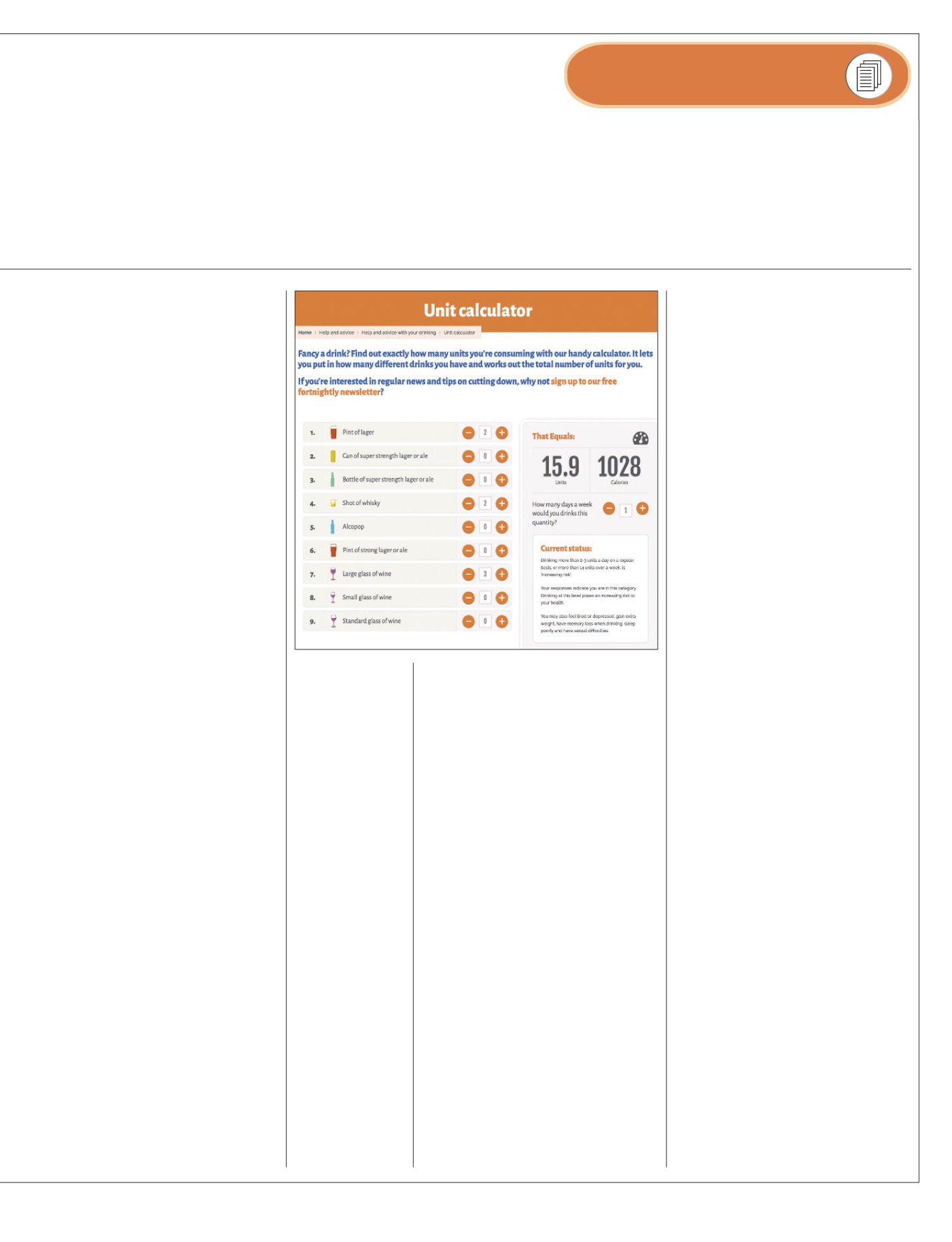
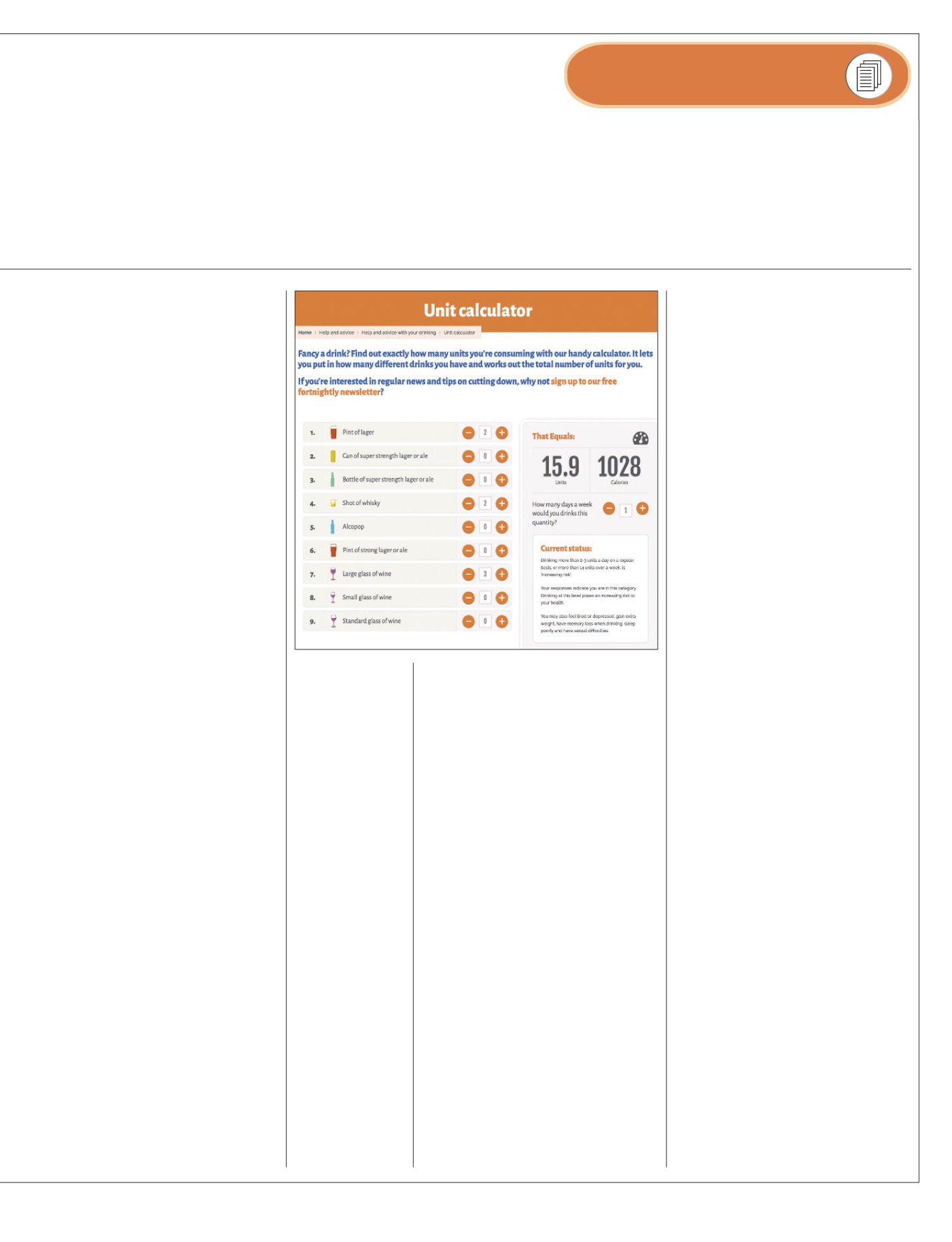
One of the major issues identified by the
report is a widespread confusion and lack of
awareness around units and guidelines. Will
the recent revisions go some way to rectifying
that or is there still a lot more to be done to
get a clearer message across? ‘In our report
nearly three quarters of respondents were
unable to correctly identify recommended
units,’ she says. ‘Hopefully the new guidelines
are a good starting point and easier to digest.
However for many people even the concept of
“units” is difficult to grasp and we may need
to work together to find better ways to
communicate the message. It would be
helpful to provide resources that allow people
to self-measure and start to understand their
own consumption better.’ The drinks industry
also needs to share a responsibility in getting
the message across, she stresses – they may
have put unit information on labels but it
‘could be a lot bigger’.
As older people have been drinking for
longer, the harm becomes accumulative, she
points out, although the fact that over-50s are
far from a homogenous group is itself a
challenge. ‘You could have an extremely fit
and healthy 73-year-old, versus a 52-year-old
with multiple health issues. We think more
discussion and exploration is required in
relation to the guidelines and how we provide
nuanced age-specific advice.’
There’s always been a strong anti-‘nanny
state’ feeling in the UK, however, and many
are likely to say, ‘If they haven’t got much else
in their lives let them enjoy a drink – why take
that away?’
‘The “nanny state” backlash is certainly
something we’re prepared for and we saw this
very much in the recent revision of the alcohol
guidelines,’ she says. ‘However we believe that
older people in particular do play an active role
in their own health and wellbeing, and given
the right information make healthier choices.
How alcohol affects us, particularly as we age,
is something most people would want to know
about in order to make this choice, in the same
way they would take care of other health areas.’
Assuming that older people don’t want to
make healthy choices or live active and
healthy lives is an ageist approach, she argues,
adding that when they do access alcohol
treatment they tend to have better outcomes
– the problem is that they’re less likely to
engage with treatment in the first place.
‘Assumptions that people are too old to
change are unhelpful and actually quite
discriminatory,’ she states.
If the aim is to help people experience a
better quality of life in their later years, a key
starting point is ‘clear and credible information’,
she stresses. ‘Many people identified positive
reasons for alcohol use such as socialising and
relaxation, and these are important factors for
people as they age. We’re not telling people not
to drink – we’re highlighting what the
particular risks are for older people and proving
advice and information.’
People have to be motivated to improve
their health, however. If someone is lonely,
perhaps bereaved, and feel they have little to
live for they may well know they’re doing
themselves harm but think, ‘So what?’What,
realistically, can be done to counter that?
‘Of course major life transitions such as
bereavement and retirement can be a trigger
for increased alcohol use, and people may feel
that there’s little in their life to change for. In
our direct engagement and support service,
where we work with people over 50 who are
already drinking problematically, our
philosophy is that it’s our job to help people
find the motivation that will help them make
that change. Very often the first stage of
engagement is about relationship building
and dealing with practical issues.’
The problem, she points out, is that it’s
resource- and time-intensive. ‘We are very
lucky to be funded so we can work in this
way,’ she says. ‘What can happen with busy
generic addiction and social work services is
resources may be stretched, and if an older
person – on the face of it – is not showing
motivation to change, resources may be
allocated elsewhere. We know that it takes
time, repeated home visits, and lots of
patience for someone to start to find their
own drive for making a change, and this is the
model we adopt.’
Equipping people with social supports and
coping strategies – ‘resilience interventions’ –
is also vital, she says, so that when they do
experience difficult life changes they are
better able to cope without turning to alcohol.
The report says that what’s needed is an
‘age-nuanced’ approach – what would some of
the elements of that look like? ‘At a wider level
there needs to be a multi-agency approach to
ensure older adults don’t fall through the net,’
she says. ‘Frontline staff and practitioners
should receive training that specifically
challenges stigma and attitudes, whilst
equipping people to better recognise and
respond to older people who may be drinking.’
Among the best-placed people to step in
are health professionals, particularly GPs, as
they’ll usually be the ones older people have
the most regular dealings with. What can be
done to raise awareness among them, and
help them spot any warning signs? ‘Health
professionals have more and more demands
on their time, but better alcohol screening of
patients is a good starting point and in some
areas this is already offered. If older patients
are re-presenting with issues such as low
mood, sleep disorders, stomach problems,
then alcohol use may be a contributing factor.
‘It also may be the case that whilst people
are not drinking at particularly high risk levels,
they are experiencing some health
implications due to age-related changes,’ she
continues. ‘It’s important for community
agencies to work closely together so that GPs
have an easy and accessible referral route
when they do identify someone.’
‘If the aim is to
help people
experience a
better quality of
life in their later
years, a key
starting point is
clear and credible
information.’
Unit calculator at
Alcohol Concern.