Basic HTML Version



June 2014 |
drinkanddrugsnews
| 21
Practice exchange|
Naloxone
www.drinkanddrugsnews.com
Sue Reynolds, the clinical
lead of substance misuse
at HMP Littlehey, tells
DDN
about joining the growing
number of prisons to
introduce a life-saving take-
home naloxone programme
for prisoners upon release
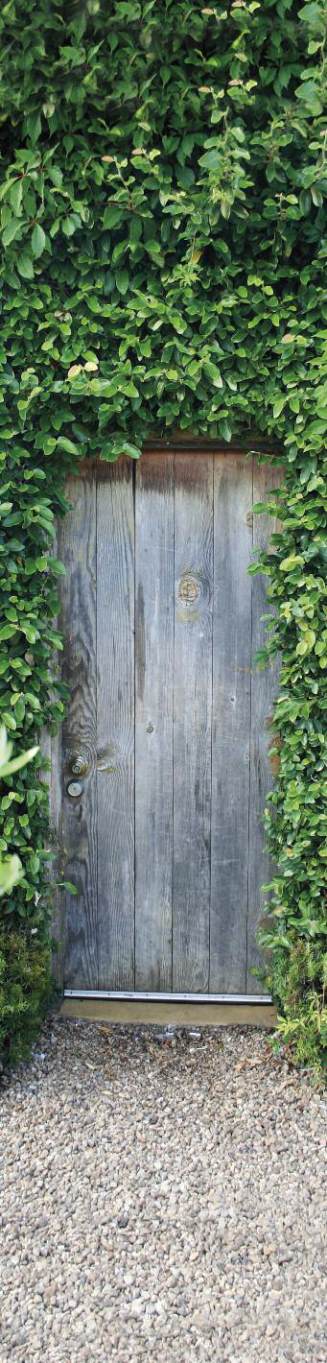
Through
The
gaTe
HMP/YOUNG OFFENDER INSTITUTE (YOI) LITTLEHEY
is
a purpose-built category C prison which holds convicted
and sentenced adults and young adults. The average
number of patients engaged in substance misuse
treatment is typically around ten to 15.
The treatment regime for substance misuse was
based on a recovery-focused approach and risks at
release for these patients were high due to social and
economic pressures, including their home situation,
family support and employment. The highest risk was
that they would have developed a low or zero tolerance
to opiates/substances as a result of having been
stabilised during custody, and so would be at an
increased risk of overdose when released.
The local service provider had initiated a take-home
naloxone programme, and so there was already support
for these patients as they returned to the community. For
these reasons, we wanted to initiate a programme within
the prison.
The task was to gain agreement from the governor of
HMP/YOI Littlehey and other senior staff for a take-home
naloxone programme to be introduced, allowing for patient
training to be undertaken and naloxone to be available ‘at
the gate’ upon release back into the community.
Initially the idea of implementing the programme was
made a reality by free training provided by Nina Bilbie, a
Prenoxad representative. The appointment was set up by
myself, with the full support of Dr Ruth Bastable, GPwSI
prescriber for substance misuse treatment. Follow up
meetings between myself, Nina and Ruth were key to
identifying and overcoming the barriers to implementation.
It turned aspiration into reality.
A needs assessment, which allowed objectives to be
clearly defined, and a working plan to ensure that all
boxes were ticked, needed to be in place. The Prenoxad
protocol was adapted to reflect what HMP/YOI Littlehey
would be delivering, and due to the small numbers, it
was agreed that a patient group directive (PGD) would
not be required and each prescription would be
generated to the named patient on an FP10 prescription.
A business plan proposal was put together, using the
support and information provided by Prenoxad, and
presented at the drugs and therapeutics/medicines
management meeting to the governor and other senior
staff, including the lead chief pharmacist managing the
prison. They were very supportive and due to the small
numbers involved, the costs were minimal, which
contributed to the positive outcome of the idea.
Training was delivered both to the clinical healthcare
staff and non-clinical, psychosocial drug and alcohol
recovery team (DART) workers in the prison, and a prison
training package for patients was also developed. A DVD
and sample syringes, needles, algorithm and instruction
packs were supplied by Prenoxad. Training was provided
by the substance misuse lead on a one-to-one basis with
the prisoner, as well as a training evaluation checklist.
It was important to ensure there was a pathway in
place for purchasing and accessing the naloxone. The
source supply is as and when required for a prisoner’s
release on an FP10 prescription, and the local pharmacist
supplies it. The naloxone is given at reception upon
release, and signed for by the prisoner and the nurse
dispensing it. A letter is also presented at the gate,
asking the prisoner to send it in if the naloxone is used
and providing information on the circumstances.
The plan has been successful due to the large amount
of people offering positive support and having the
motivation to take it forward. The key factor was that
shared expertise was available and easily accessible. The
same commissioners (the DAAT) who provide the
Inclusion programme both within the prison and the local
community also commission and provide the clinical
substance misuse treatment services in the prison. The
GPwSI working within the prison also provides for the
local community, and all key players involved were in
agreement for the plan to be implemented. This was
running concurrently with the community service providers
who were initiating the same implementation plan.
There were no huge obstacles or barriers to
overcome, as the support was there from the head of
healthcare, the governor and the chief pharmacist. The
materials provided by Prenoxad were excellent and
enabled things to happen very quickly, while the protocol
was easily adapted to reflect local practice.
The patients thought it was an excellent idea – they
were very keen and appreciative that this was available
to them and it made them feel empowered and
supported. It has been included in the programme
delivered on the drug recovery wing as part of the first
aid and overdose session, and the prisoners who have
had training have felt it has boosted their confidence in
being able to manage an opioid overdose situation.
To be able to have naloxone injections available for
prisoners being released is a huge breakthrough for
drug treatment intervention in the prison setting. It
takes away some of the worry of releasing vulnerable
people into the community with a high risk of overdose.
It has been a fantastic achievement and I was provided
with tremendous support from colleagues. I hope this
initiative continues to spread nationwide with little
resistance – if it is available in the community, it can be
made available within secure settings too.
‘There were no huge
obstacles or barriers to
overcome, as the support
was there from the head of
healthcare, the governor
and the chief pharmacist.’
SUE REYNOLDS

